Understanding Vagina Prolapse (Pelvic Organ Prolapse)
Causes, Symptoms, and Treatment Options for Women's Pelvic Health
Vagina Prolapse (Pelvic Organ Prolapse) is a condition that affects many women, particularly those who have given birth or are experiencing menopause. Despite its prevalence, it is often under-discussed, leading to a lack of awareness and understanding.
What is Vagina Prolapse (Pelvic Organ Prolapse)?
Vagina Prolapse (Pelvic Organ Prolapse), also known as pelvic organ prolapse (POP), occurs when the pelvic floor muscles and ligaments supporting the pelvic organs weaken or stretch, causing one or more organs to descend into or even outside the vaginal canal. These organs may include the uterus, bladder, rectum, or the vagina itself.
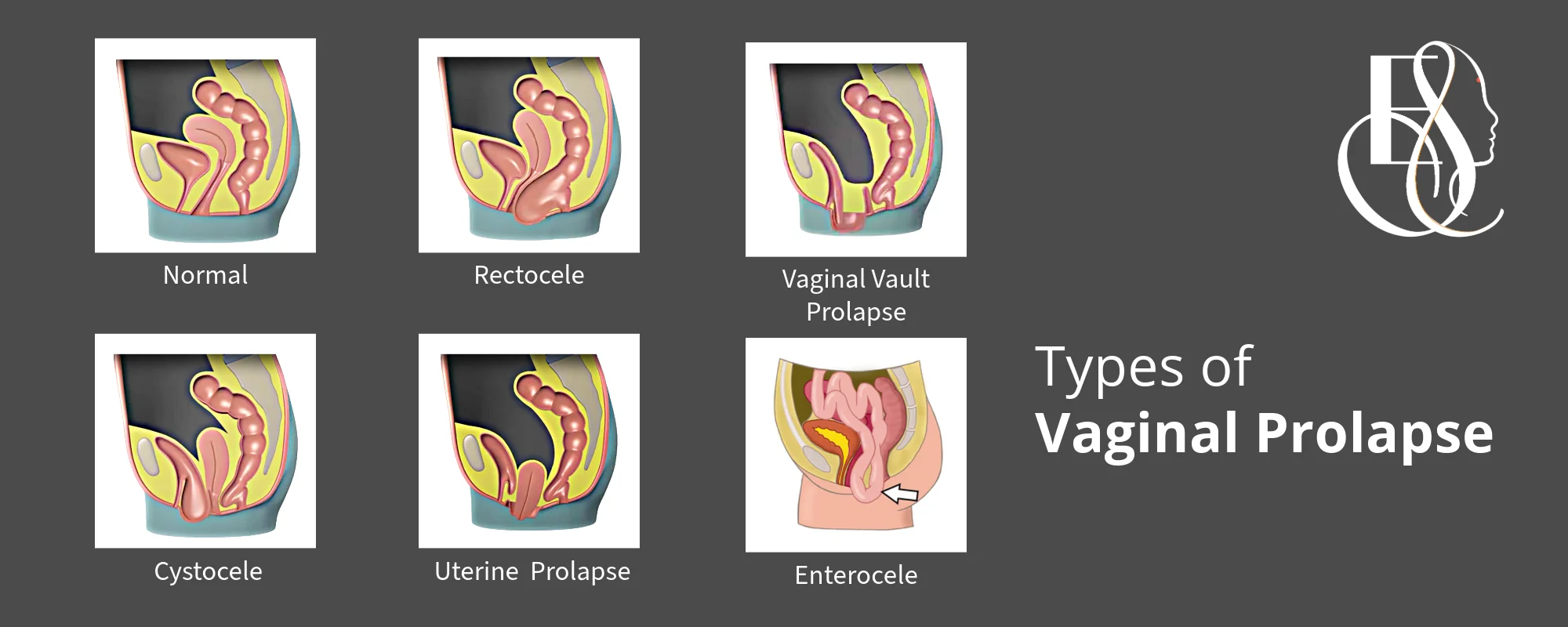
The severity of prolapse can range from mild to severe, with varying degrees of impact on a woman’s quality of life. Types of Vaginal Prolapse:
- Cystocele (Anterior Prolapse): The bladder drops into the vagina. This is the most common type of female prolapse, in which the ttissue supporting the bladder stretches or detatches and may sink against the front wall of the vagina. It may result in difficulty in passing uring, pain during sex, incontinence or general discomfort.
- Rectocele (Posterior Prolapse): The rectum bulges into the vagina. It happens in women whos posterior ( back) wall of the vagina is weakened. In severe cases the bulge may tear into the vagina. This may result in rectal pain, constipation, a feeling of pressure in the rectum or sometimes a woman may feel that the bowel hasnt been emptied even after finishing her bowel movement.
- Uterine Prolapse: As the name suggests, it means the uterus descends into the vagina or may even protrude outside the vagina. The uterus is a powerful, muscular organ that stretches during childbirth and pregnancy, but a dropped uterus can cause quite a few problems. It may lead to other prolapses on this list, as the weight of this organ puts pressure on other weakened organs, causing them to sink. A uterine prolapse, if it goes completely unaddressed and untreated, can painfully protrude outside of the vagina in a disorder called procidentia. A prolapsed uterus can feel like you’re sitting on a ball, lead to beading and may lead to pain during sex.
- Vaginal Vault Prolapse: The top of the vagina drops down after a hysterectomy. Because the uterus has been removed, nothing is anchoring the top of the vagina or cervix in place, and it may sometimes sink. In very severe cases, the vagina may fall through the opening.
- Enterocele: The small intestine pushes against the vaginal wall.In some cases, the small bowel, or small intestine may sink into the lower pelvic cavity, affecting the top part of the vagina.
Vaginal Prolapse Elle Sante Reconstructive Cosmetic Gynaecology
What are the causes of Vagina Prolapse (Pelvic Organ Prolapse) ?
Understanding the underlying causes of vaginal prolapse is crucial for prevention and treatment. Some of the primary factors contributing to this condition include:
- Pregnancy and Childbirth: The strain of pregnancy and vaginal delivery can weaken pelvic floor muscles and damage supporting tissues.
- Aging and Menopause: As women age, especially after menopause, the natural decline in estrogen levels can lead to weakened pelvic floor muscles and tissues.
- Chronic Stress: Conditions that cause frequent coughing, sneezing, or straining during bowel movements can put excessive pressure on the pelvic floor.
- Obesity: Excess body weight increases pressure on the pelvic organs and can weaken supporting structures.
- Hysterectomy: Removal of the uterus can sometimes lead to weakened pelvic floor support.
- Genetics: Some women may be genetically predisposed to weaker connective tissues.
- Heavy Lifting: Regularly lifting heavy objects can strain the pelvic floor muscles over time.
Who are at risk to have Vagina Prolapse (Pelvic Organ Prolapse) ?
Any woman can develop Vaginal Prolapse. However, the women who are at higher risk include women:
- With multiple vaginal deliveries
- Who had Large birth weight babies
- Who had Prolonged labor during childbirth
- On whom assisted devices (forceps or vacuum) were used during delivery
- With family history of pelvic floor disorders
- With Chronic constipation or straining during bowel movements
- With Chronic cough (e.g., from smoking or respiratory conditions)
- With Connective tissue disorders (e.g., Ehlers-Danlos syndrome)
- Doing High-impact activities or heavy lifting
- Who have history of Pelvic surgery, including hysterectomy
- Who are overweight, and the excess weight puts additional pressure on the pelvic floor.
What are the symptoms of Vagina Prolapse (Pelvic Organ Prolapse) ?
Recognizing the symptoms of vaginal prolapse is essential for early diagnosis and treatment. Common signs and symptoms include:
- A feeling of fullness or pressure in the pelvic area
- A sensation of something “falling out” of the vagina
- Difficulty urinating or having a bowel movement ( constipation )
- Urinary incontinence or frequent urination
- Pain or discomfort during sexual intercourse
- Lower back pain that eases when lying down
- Visible or palpable tissue protruding from the vagina
- Difficulty inserting or keeping tampons in place
- Recurring bladder infections
- A pulling or stretching sensation in the groin area
What is the Impact of Vagina Prolapse (Pelvic Organ Prolapse) on Women's Lives ?
Vaginal prolapse can significantly affect a woman’s quality of life, both physically and emotionally. Some of the ways it can impact daily living include:
- Physical Discomfort: Persistent pain or pressure in the pelvic area can interfere with daily activities and exercise.
- Sexual Function: Pain or discomfort during intercourse can lead to decreased sexual satisfaction and intimacy issues.
- Urinary and Bowel Problems: Difficulty urinating or having bowel movements can cause frustration and embarrassment.
- Emotional Distress: Feelings of self-consciousness, anxiety, or depression may arise due to the physical symptoms and their impact on daily life.
- Body Image: The visible or palpable changes in the vaginal area can affect a woman’s body image and self-esteem.
- Social Isolation: Women may limit social activities due to discomfort or fear of embarrassing symptoms.
- Work Performance: Discomfort and frequent trips to the bathroom can affect productivity and job satisfaction.
- Exercise Limitations: Some women may avoid certain physical activities due to discomfort or fear of worsening the prolapse.
Seeking treatment for vaginal prolapse is crucial for several reasons:
- Symptom Relief: Proper treatment can alleviate discomfort and improve quality of life.
- Prevention of Progression: Early intervention can help prevent the condition from worsening.
- Improved Urinary and Bowel Function: Treating prolapse can address associated urinary and bowel issues.
- Enhanced Sexual Function: Addressing prolapse can improve sexual comfort and satisfaction.
- Emotional Well-being: Successful treatment can boost self-esteem and reduce anxiety related to the condition.
- Preservation of Pelvic Organ Function: Timely treatment can help maintain the proper function of pelvic organs.
- Avoidance of Complications: Untreated severe prolapse can lead to ulceration, infection, or urinary retention.
How is Vagina Prolapse (Pelvic Organ Prolapse) Diagnosed ?
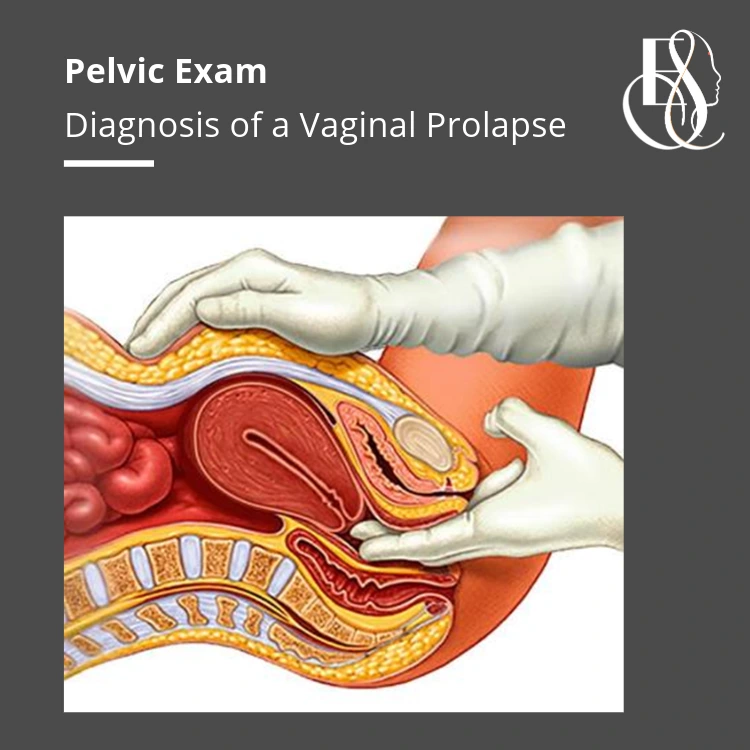
Basis the above symptoms, a woman should self evaluate the problem. You should go to a specialized Reconstructive and Cosmetic Gynaecologist, who is skilled in a an array of non surgical and surgical treatments for Vaginal Prolapse.
Diagnosing vaginal prolapse typically involves a pelvic examination by a reconstructive and cosmetic gynaecologist. A Pelvic exam is a physical checkup by a skilled healthcare professional. It involves check up of a female’s reprodutive and urinary tract. The doctor is able to guage signs of disease by physically touch and feel of the organs surrounding the vaginal canal.
During a pelvic exam, especially to evaluate vaginal prolapse, the doctor will ask the patient to bear some pressure down similar to having a bowel movement. This helps them observe signs and extrent of a prolapse. After a preliminary pelvic exam the doctor will order additional tests, to medically understand the size and extent of the condition. Urodynamic tests or imaging studies, may be necessary to evaluate the severity of the prolapse and to plan appropriate treatment.
What are the Treatment Options for Vagina Prolapse (Pelvic Organ Prolapse) ?
Non-Surgical Treatment Options
For mild to moderate cases of vaginal prolapse, non-surgical treatments can be effective. Women often prefer to alleviate their prolapse conditions and relieve symptoms through non invasive procedures. These are very effective in improvement of quality of life if done consistently and as per a professional’s advise.
- Lifestyle Changes: Maintaining a healthy weight, avoiding heavy lifting, and managing chronic cough or constipation can help reduce symptoms.
- Pelvic Floor Exercises (Kegels): These exercises strengthen the pelvic floor muscles, providing better support for the pelvic organs. Consistent practice can improve symptoms and prevent worsening of the prolapse. Kegels are performed by women by contracting and relaxing their pelvic muscles, similar to the feeling of holding and releasing of urine. They are very easy to do and can be done virtually anywhere and anytime. While Kegel excersises help in some improvement of symptoms, they may take a long time to show effect.
- Pessary Devices: A pessary is a silicone device inserted into the vagina to support the pelvic organs. It can be a good option for women who are not candidates for surgery or prefer to avoid it.
Surgical Treatment Options
In cases where non-surgical treatments are insufficient, surgical options may be necessary. These procedures aim to restore the normal anatomy of the pelvic organs. A skilled reconstructive & cosmetic Gynaecologist wil be able to understand the severity and the exact nature of the prolapse. After thorough diagnosis, the doctor will explain the type of surgical intervention needed to resolve the issue.
- Vaginal Repair Surgery: This surgery involves repairing the vaginal walls to provide better support for the prolapsed organs. It can be performed through the vagina, resulting in minimal scarring.
- Laparoscopic Repair Surgery: This minimally invasive surgery uses small incisions and specialized instruments to repair the prolapse. It offers quicker recovery times and less post-operative pain compared to traditional surgery.
Vaginal Prolapse, unfortunately, is very difficult to reverse if it has passed the threshold of a mild stage. Also, it can keep worsening with age and day-to-day activities, sometimes brining all normal life to a standstill. So, it is always better to take a consultation on your condition at the very first onset of symptoms of vaginal prolapse.
Frequently Asked Questions
Can vaginal prolapse heal on its own?
Is vaginal prolapse a normal part of aging?
Can I still have sex with vaginal prolapse?
Will I need surgery for vaginal prolapse?
Can I get pregnant with vaginal prolapse?
How long is the recovery from prolapse surgery?
Can vaginal prolapse recur after treatment?
Are there any natural remedies for vaginal prolapse?
While not cures, pelvic floor exercises and lifestyle changes can help manage symptoms in mild cases.
Can young women develop vaginal prolapse?
Vaginal prolapse is a common condition that many women face, but it doesn’t have to control your life. By understanding the symptoms, risk factors, and available treatments, you can take proactive steps to manage and treat this condition. Whether you opt for lifestyle changes, non-surgical treatments, or surgical solutions, the key is to stay informed and work closely with your reconstructive and cosmetic gynaecologist. Empowering yourself with knowledge and taking charge of your health is the first step towards a better quality of life.
By providing this comprehensive guide, we, at Elle Sante hope to shed light on vaginal prolapse and help women feel more confident and informed about their health choices.
The sense of vaginal prolapse can be very overwhelming for a woman. It not only affects her day-to-day life but also her mental well being. Taking precautions is just not enough. It is critical that you consult a reconstructive & cosmetic gynaecologist soon. The specialist is able to guage the severity of the condition and with his expertise able to create a personalized treatment plan for the paitent which is most appripriate towards best patient outcomes. Dr Navneet Magon has over 30 years of expertise in treating women pelvic area conditions from mild to severe. He has delivered over 25000 procedures at varying level of severity. Take a consultation from Dr Navneet Magon on your case.
Discuss your queries on Vagina Prolapse (Pelvic Organ Prolapse)
-
+91-8811 009 900+91-8811 009 900
-
WhatsApp Us (24/7)WhatsApp Us (24/7)
Mon-Sat 10:30am to 7:30pm
Sunday Closed
-
info@ellesante.ininfo@ellesante.in
We respond within 24 hours
Contact Us
Elle Sante Range of Treatments
Elle Sante Clinics







Elle Sante Gurgaon
NR – 38, Main, Nathupur Rd, DLF Phase 3, Sector 24, Gurugram, Haryana 122002
Elle Sante Mumbai
6th floor, S.M House, 11, Sahakar Rd, Vishnu Prasad Society, Navpada, Vile Parle East, Vile Parle, Mumbai, Maharashtra 400057
Elle Sante Hyderabad
C/o FMS Sculpt & Dental Hospital Door No. 8-2-293/82/A/725, Road No. 37, Hitech City Rd, nr Daspalla Hyderabad, CBI Colony, Jubilee Hills, Hyderabad, Telangana 500033
Elle Sante Visakhapatnam
Health city, Medcy Hospitals, Plot 9A, chinagadili, Arilova, Visakhapatnam, Andhra Pradesh 530040
Elle Sante Agra Pratappura Centre
Khandelwal Nursing Home, 3/27, Mahatma Gandhi Rd, khandelwal Colony, Pratap Pura, Rakabganj, Agra, Uttar Pradesh 282001
Elle Sante Rohtak
Elle Sante Nursing Home, C/o, Civil Rd, opposite Piller No. 22, HUDA Complex, Rohtak, Haryana 124001
Elle Sante Firozabad
Om Hospital and Research Centre, SN Rd, opposite PK Tiles, Devnagar, Nai Basti, Firozabad, Uttar Pradesh 283203
Elle Sante Agra
3rd Floor, Shanti Madhuban Plaza, 1/2, Delhi Gate Rd, Hariparwat, Professors Colony, Civil Lines, Agra, Uttar Pradesh 282002